| Login | ||

Healthcare Training Institute - Quality Education since 1979
CE for Psychologist, Social Worker, Counselor, & MFT!!
Section 1
Medication Errors: Definitions, Classifications, Root Causes
Question 1 | Test | Table of Contents
Thoughts on How to Avoid Medical Errors
There are many frustrations and difficulties in our stressful careers. In my experience the best way to avoid medical errors is with support. Here is a list of ways that mental health professionals can avoid making medical errors.
1.Computer programs - Nowadays there are cost cutting computer programs for scoring psychological tests such as the MMPI-2 and MMPI-A. This prevents the possibility of human error in scoring a test.
2.Typist - If you are able to work full time and/or can afford a typist to edit your work, records, and insurance/billing forms this is very helpful.
3.Sufficient time with tests to ensure proper scoring - Also we are always under pressure to be super doctors and are pressured by parents, for example, to rush educational tests and reports. This usually happens at the end of semesters or when the child is going to be retained. In order to prevent errors in test results, mental health professionals need to make sure that they do not give into this pressure and spend sufficient time administering, scoring, and interpreting tests.
4.Determining lies in custody and court cases - Custody and criminal litigation are a landmine of lies about crimes, partners, false allegations of sexual abuse in the former, adversarial lawyers etc. It is important to find the truth in custody and criminal litigations.
5.Avoiding manipulation of lawyers - Never let a lawyer manipulate you about your testimony or cross examination will be a nightmare.
6.Set limits on what you can realistically get done - If you are going through a difficult life situation set limits of what can be done.
7. Insurance Claims - HMOS and PPOs put one in a no win situation about providing quality care, maintaining confidentiality, getting authorizations, and then trying to get paid. Be careful when dealing with HMOs and PPOs.
Medication errors: definitions and classification
All of these methods have been adduced by Aronson and Ferner in their approach to defining terms relevant to drug safety terminology [14] and medication errors [15] and by Hauben and Aronson in defining the term ‘signal’ in pharmacovigilance [16]. I shall not reiterate all the arguments here.
A medication
Like many terms of this form (e.g. ‘definition’, ‘prescription’), ‘medication’ can mean either a process or an object that undergoes the process. A medication (the object) can be considered to be the same as a medicinal product, which has been defined in terms of what a medicinal product is and what it does. Thus, a medication is ‘[a product that] contains a compound with proven biological effects, plus excipients, or excipients only; it may also contain contaminants; the active compound is usually a drug or prodrug, but may be a cellular element’ [14]. There is a codicil to this definition, which is not strictly part of the definition, but describes certain attributes of a medicinal product.
The codicil stipulates that a medicinal product is one that is intended to be taken by or administered to a person or animal for one or more of the following reasons: as a placebo; to prevent a disease; to make a diagnosis; to test for the possibility of an adverse effect; to modify a physiological, biochemical, or anatomical function or abnormality; to replace a missing factor; to ameliorate a symptom; to treat a disease; to induce anesthesia. Medication (the process) is the act of giving a medication (the object) to a patient for any of these purposes. This definition reminds us of the distinction between the drug itself (the active component) and the whole product.
It includes chemical compounds, either drugs or prodrugs (which themselves may have no pharmacological activity), or, in racemic mixtures, stereoisomers that may have only adverse effects, or compounds that are used for diagnostic purposes (such as contrast media); it also includes cellular elements, such as inactivated or attenuated viruses for immunization, blood products (such as erythrocytes), viruses for gene therapy, and embryonic stem cells; ‘contaminants’ includes chemical and biological contaminants and adulterants, the former being accidentally present, the latter deliberately added. Thus, the definition covers a wide range of compounds. However, it does not include medications when they are used to probe systems for nondiagnostic purposes, such as the use of phenylephrine to study baroreceptor reflexes in a physiological or pharmacological experiment.
An error
An error is ‘something incorrectly done through ignorance or inadvertence; a mistake, e.g. in calculation, judgment, speech, writing, action, etc.’ [1] or ‘a failure to complete a planned action as intended, or the use of an incorrect plan of action to achieve a given aim’ [17]. Other definitions have been published [18].
A medication error
With these definitions in mind, a medication error can be defined as ‘a failure in the treatment process that leads to, or has the potential to lead to, harm to the patient’ [15].The use of the term ‘failure’ signifies that the process has fallen below some attainable standard. The ‘treatment process’ includes treatment for symptoms or their causes or investigation or prevention of disease or physiological changes. It includes not only therapeutic drugs but also the compounds referred to above. It also includes the manufacturing or compounding, prescribing, transcribing (when relevant), dispensing, and administration of a drug, and the subsequent monitoring of its effects.
‘Harm’ in the definition also implies ‘lack of benefit’, a form of treatment failure. Note that the definition does not specify who makes the error – it could be a doctor, a nurse, a pharmacist, a career, or another; nor does it specify who is responsible for preventing errors. Different definitions of medication errors have been tested, as all technical definitions should be. In this case it was done by devising scenarios and determining which would constitute an error under each of the definitions.
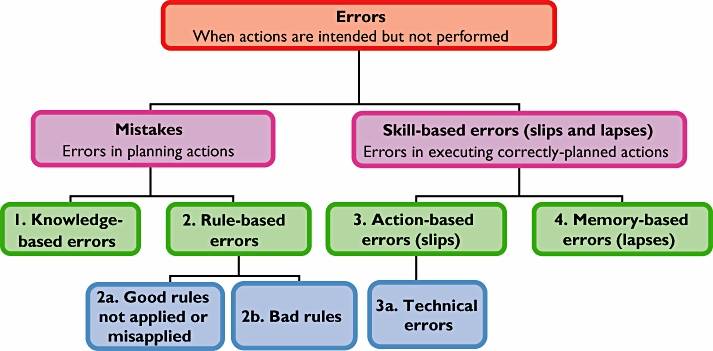 Figure 1 - The classification of medication errors based on a psychological approach (reproduced from reference 15, with permission from Wolters Kluwer Health/ Adis©; Adis Data Information BV (2006); all rights reserved)
Figure 1 - The classification of medication errors based on a psychological approach (reproduced from reference 15, with permission from Wolters Kluwer Health/ Adis©; Adis Data Information BV (2006); all rights reserved)
Classification of medication errors
The best way to understand how medication errors happen and how to prevent them is to consider their classification, which can be contextual, modal, or psychological. Contextual classification deals with the specific time, place, medicines, and people involved. Modal classification examines the ways in which errors occur (e.g. by omission, repetition, or substitution). However, classification based on psychological theory [21] is to be preferred, as it explains events rather than merely describing them. Its disadvantage is that it concentrates on human rather than systems sources of errors. These classifications have been discussed in detail elsewhere [15].
Psychologists consider an error to be a disorder of an intentional act, and they distinguish between errors in planning an act and errors in its execution. If a prior intention to reach a specified goal leads to action, and the action leads to the goal, all is well. If the plan of action contains some flaw, that is a ‘mistake’. If a plan is a good one but is badly executed, that is a failure of skill. This approach yields four broad types of medication error (numbered 1–4 in Figure 2) [15, 22].Mistakes can be divided into (i) knowledge-based errors and (ii) rule-based errors. Failures of skill can be divided into (iii) action-based errors (’slips’, including technical errors) and (iv) memory based errors (‘lapses’).
Knowledge-based errors can be related to any type of knowledge, general, specific, or expert. It is general knowledge that penicillin can cause allergic reactions; knowing that your patient is allergic to penicillin is specific knowledge; knowing that co-fluampicil contains penicillin is expert knowledge. Ignorance of any of these facts could lead to a knowledge-based error.
Rule-based errors can further be categorized as (a) the misapplication of a good rule or the failure to apply a good rule; and (b) the application of a bad rule. An action-based error is defined as ‘the performance of an action that was not what was intended’ [23]. A slip of the pen, when a doctor intends to write diltiazem but writes diazepam, is an example.
Technical errors form a subset of action-based errors. They have been defined as occurring when ‘an outcome fails to occur or the wrong outcome is produced because the execution of an action was imperfect’ [24]. An example is the addition to an infusion bottle of the wrong amount of drug [25]. Memory-based errors occur when something is forgotten; for example, giving penicillin, knowing the patient to be allergic, but forgetting.
Preventing errors through classification
This classification can help understand how errors can be prevented, as discussed in detail elsewhere [15]. Knowledge-based errors can obviously be prevented by improving knowledge, e.g. by ensuring that students are taught the basic principles of therapeutics [26, 27] and tested on their practical application [28] and that prescribers are kept up to date. Computerized decision-support systems can also train prescribers to make fewer errors [29, 30]. Mistakes that result from applying bad rules, or misapplying or failing to apply good rules (rule-based errors) can be prevented by improving rules. Training can help in preventing technical (action based) errors. Memory-based errors are the most difficult to prevent. They are best tackled by putting in place systems that detect such errors and allow remedial actions. Check lists and computerized systems can help.
Conclusion
Medication errors, which can lead to adverse drug reactions, require clear and unambiguous definitions, so that patients, prescribers, manufacturers, and regulators can all understand each other. The classification of medication errors on the basis of the underlying psychological mechanisms, based on how errors occur, can suggest strategies that help to reduce their occurrence.
--Aronson, J. K. (2009). Medication errors: definitions and classification. British Journal Of Clinical Pharmacology, 67(6), 599-604. doi:10.1111/j.1365-2125.2009.03415.x
Personal
Reflection Exercise Explanation
The
Goal of this Home Study Course is to create a learning experience that enhances
your clinical skills. We encourage you to discuss the Personal Reflection
Journaling Activities, found at the end of each Section, with your colleagues.
Thus, you are provided with an opportunity for a Group Discussion experience.
Case Study examples might include: family background, socio-economic status, education,
occupation, social/emotional issues, legal/financial issues, death/dying/health,
home management, parenting, etc. as you deem appropriate. A Case Study is to be
approximately 75 words in length. However, since the content of these “Personal
Reflection” Journaling Exercises is intended for your future reference, they
may contain confidential information and are to be applied as a “work in
progress.” You will not
be required to provide us with these Journaling Activities.
Personal
Reflection Exercise #1
The preceding section contained information
about medical errors. Write one case study examples
regarding how you might use the content of this section in your practice.
Reviewed 2023
Update
Medication Dispensing Errors and Prevention
Tariq, R. A., Vashisht, R., Sinha, A., & Scherbak, Y. (2023). Medication Dispensing Errors and Prevention. In StatPearls. StatPearls Publishing.
Peer-Reviewed Journal Article References:
McGrath, R. E. (2020). What is the right amount of training? Response to Robiner et al. Clinical Psychology: Science and Practice, 27(1), Article e12315.
Robiner, W. N., Tompkins, T. L., & Hathaway, K. M. (2020). Prescriptive authority: Psychologists’ abridged training relative to other professions’ training. Clinical Psychology: Science and Practice, 27(1), Article e12309.
Shahidullah, J. D., Hostutler, C. A., & Forman, S. G. (2019). Ethical considerations in medication-related roles for pediatric primary care psychologists. Clinical Practice in Pediatric Psychology, 7(4), 405–416.
QUESTION 1
What are the four broad types of Medication Errors? To select and enter your answer go to Test.
Test
Section 2
Table of Contents
Top
Excerpts from Bibliography referenced in this article
1. Oxford English dictionary [online]. Available at http://ezproxy.ouls.ox.ac.uk:2118/entrance.dtl (last accessed 2 February 2009).
14. Aronson JK, Ferner RE. Clarification of terminology in drug safety. Drug Saf 2005; 28: 851–70.
15 Ferner RE, Aronson JK. Clarification of terminology in medication errors: definitions and classification. Drug Saf 2006; 29: 1011–22.
16. Hauben M, Aronson JK. Defining ‘signal’ and its subtypes in pharmacovigilance based on a systematic review of previous definitions. Drug Saf 2009; 32: 99–110.
17. Kohn L, Corrigan J, Donaldson M, eds. To Err is Human: Building a Safer Health System.Washington DC: Institute of Medicine, 1999.
18. Yu KH, Nation RL, Dooley MJ. Multiplicity of medication safety terms, definitions and functional meanings: when is enough enough? Qual Saf Health Care 2005; 14: 358–63.
21. Reason JT. Human Error. New York: Cambridge University Press, 1990.
22. Ferner RE, Aronson JK. Errors in prescribing, preparing, and giving medicines – definition, classification, and prevention. In: Side Effects of Drugs, Annual 22, ed. Aronson JK. Amsterdam: Elsevier, 1999; xxiii–xxxvi.
23. Norman DA. Categorization of action slips. Psychol Rev 1981; 88: 1–15.
24. Runciman WB, Sellen A,Webb RK, Williamson JA, Currie M, Morgan C, Russell WJ. The Australian incident monitoring study. Errors, incidents and accidents in anaesthetic practice. Anaesth Intensive Care 1993; 21: 506–19.
25. Ferner RE, Langford NJ, Anton C, Hutchings A, Bateman DN, Routledge PA. Random and systematic medication errors in routine clinical practice: a multicentre study of infusions, using acetylcysteine as an example. Br J Clin Pharmacol 2001; 52: 573–7.
26. Maxwell S,Walley T. Teaching safe and effective prescribing in UK medical schools: a core curriculum for tomorrow’s doctors. Br J Clin Pharmacol 2003; 55: 496–503.
27. Likic R,Maxwell SRJ. Prevention of medication errors: teaching and training. Br J Clin Pharmacol 2009; 67: 656–61.
28. Langford NJ, Landray M,Martin U, Kendall MJ, Ferner RE. Testing the practical aspects of therapeutics by objective structured clinical examination. J Clin Pharmacol Ther 2004; 29: 263–6.
29. Anton C, Nightingale PG, Adu D, Lipkin G, Ferner RE. Improving prescribing using a rule based prescribing system. Qual Saf Health Care 2004; 13: 186–90.
30. Agrawal A.Medication errors: prevention using information technology systems. Br J Clin Pharmacol 2009; 67: 681–6.

